The effects of estradiol on human in the brain are unclear. Currently, there are no hormone markers within the brain to determine the association of levels of sex hormones with libido. In clinical studies, we make a presumption that serum estradiol reflects brain estradiol levels or activity. It may be possible that if serum estradiol level is low that more estradiol is then more is available for the brain, as it is shifted from the rest of the body to the brain. This hypothesis is given to support the results of a study we did previously, of not associating low libido to higher estradiol levels. In one of our previous studies, positive emission tomography (PET) was used in an attempt to map areas of the brain involved in glucose metabolism after administration of testosterone. The brain stem and parietal lobes were highly metabolic, suggesting these areas involved in sexual processing. There are current arguments for an optimal T: E2 ratio for sexuality, rather than the actual amount, but studies are generally weakly powered.
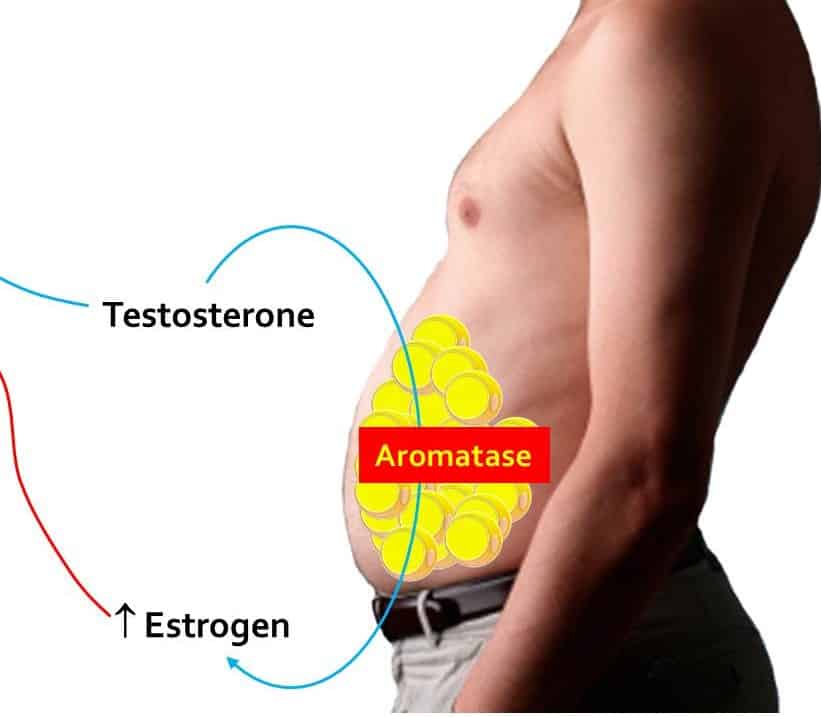
As mentioned, not much work has been done to better understand the role of estrogens in men. There has also been a distinction between work done on endogenous estrogens and also exogenous estrogens, be it given as estrogen itself or converted from testosterone. In one of our studies, we tried to understand the characteristics of exogenous estrogens which in this case are aromatized from exogenous testosterone given to treat hypogonadism. It appeared that age may be a determinant of the conversion of testosterone to estrogens, except for later years in life after 65 years old. The clinical importance of high estrogen after TRT continues to be debated. We found that high estrogen after TRT does not necessarily associate with low libido.
We have noticed that AI and SERM were prescribed frequently by doctors to lower estrogen in men. There are challenges in setting up a guideline for the threshold beyond which AI and SERM are to be used, as there are no evidence based studies at this time to guide the practice. Normality based on standard deviation can be used, but we found that age in itself may cause variations in normal values. Although our study did not associate low libido with high E2 levels; there could be hypothetical challenges to exposure to high estrogen over a longer period of time We think that the use of AI and SERM should be individualized and carefully monitored. The common side effects of AIs include constipation,, diarrhea, nausea, vomiting, upset stomach, loss of appetite, body aches and pains, breast swelling/tenderness/pain, headache, dry mouth, scratchy throat, increased cough, dizziness, trouble sleeping, tiredness/weakness, flushing and sweating (hot flashes/hot flushes), hair thinning, and weight change should be communicated to the patent. Changes in diet such as eating several small meals may help lessen the chance of nausea and vomiting. More work such as a longitudinal, controlled study is needed to assess the role of exogenous estrogens from TRT and the need to treat this condition.

