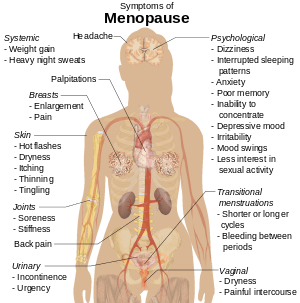
During a woman’s reproductive years, the ovaries produce estrogen and progesterone. Estrogen is important for normal menstrual periods and fertility, and it promotes bone strength. Estrogen and progesterone levels drop substantially during menopause. In some women (not all women) it may cause symptoms such as hot flashes.
Postmenopausal hormone therapy is the term used to describe the two hormones, estrogen and progesterone, that are often given to relieve menopausal symptoms. In general, for women whose womb has been removed, estrogen alone can be given.
For those with intact wombs, both estrogen and progesterone (synthetic or natural/ bioidentical/ BHRT ) are given. Estrogen is the most effective treatment available to relieve bothersome symptoms of menopause. However, some women cannot take estrogen- such as those with breast cancer or recent thrombosis. Sometimes, women choose not to take hormone therapy and prefer herbal solutions. Indeed, there are some alternatives to hormone therapy to treat menopausal symptoms. Although they may not be as effective as estrogen, they do provide some relief.
What are non-hormonal alternatives to control Hot Flashes?
Non-estrogen treatments for hot flashes are effective in many women. In general, none work as well as estrogen or progesterone, but they are better than placebo (sugar pills). However, not all women need treatment for hot flashes since they are mild in some women.
These are some examples of other choices:
Paroxetine — Paroxetine (Brisdelle/Paxil) is the only non-hormonal therapy that is specifically approved for hot flashes in the US by the FDA. This agent has been used for many years for depression but can be taken at a lower dose for hot flashes.
Gabapentin — Gabapentin (Neurontin) is a drug that is primarily used to treat seizures. It also relieves hot flashes in some women, preferably given as a single bedtime dose or during the daytime as well.
Antidepressants — Antidepressant medications are recommended as a first line treatment for hot flashes in women who cannot take estrogen. Paroxetine (Paxil) is the only drug approved in the United States for hot flashes in this class, but each of these agents has been used for hot flashes.
- Venlafaxine (brand name: Effexor), citalopram (brand name: Celexa), and escitalopram (brand name: Lexapro) were developed to treat depression, but studies show that they are an effective treatment for hot flashes. Paroxetine (sample brand name: Paxil) is also effective for hot flashes, but you should not take paroxetine if you have breast cancer and are taking tamoxifen. The worry is that paroxetine can interfere with tamoxifen and make it less effective.
- Fluoxetine (brand name: Prozac) and sertraline (brand name: Zoloft) do not work as well as the other antidepressants listed.
Progesterone — The injectable progestin birth control hormone medroxyprogesterone acetate (brand name: Depo-Provera) helps to reduce hot flashes but is uncommonly used. Also, natural progesterone (obtained from yam) can be prepared through compounding. In our practice, this is generally preferred over the synthetic version.
Plant-derived estrogens (phytoestrogens) — Plant-derived estrogens have been marketed as a “natural” or “safer” alternative to hormones for women with menopausal symptoms. Phytoestrogens are found in many foods, including soybeans, chickpeas, lentils, flaxseed, lentils, grains, fruits, vegetables, and red clover. Isoflavone supplements, a type of phytoestrogen, can be purchased in health food stores.
However, it is uncertain whether phytoestrogens help to reduce hot flashes or night sweats; most studies have not reported benefit. In addition, some phytoestrogens might act like estrogen in some tissues of the body. Many experts suggest that women who have a history of breast cancer should avoid phytoestrogens.
Herbal treatments — A number of herbal treatments have been promoted as a “natural” remedy for hot flashes. In fact, many postmenopausal women use black cohosh for hot flashes, but clinical trials have shown that it is not more effective than placebo. In addition, there are safety concerns about some herbs, including black cohosh, which might stimulate breast tissue (similar to estrogen). Herbal treatments are not recommended for hot flashes or other menopausal symptoms.
What about treating Vaginal Dryness?
Low-dose vaginal estrogen in the form of a suppository is a very effective treatment for postmenopausal women with vaginal dryness or pain with intercourse. This is a treatment that women can continue for many years after menopause because only minimal amounts get into the bloodstream. On this basis, low-dose estrogen is not thought to increase the risk of breast cancer, heart attack, or stroke.
If you are looking for expert advice on how to manage your menopausal symptoms in Houston, Texas, consider the Opal Medical Clinic. You can find out more information on us at www.opalmedical.com

